This is what APTAMD does best.
We advocate to protect the PT profession, practice and patients. Join us Feb 7 in Annapolis -without your voices and participation prior auth reform doesn’t happen.
APTAMD and 56 other health occupations have drafted legislation with insurers to reduce delays and administrative burden. We will have a bill number later this month.
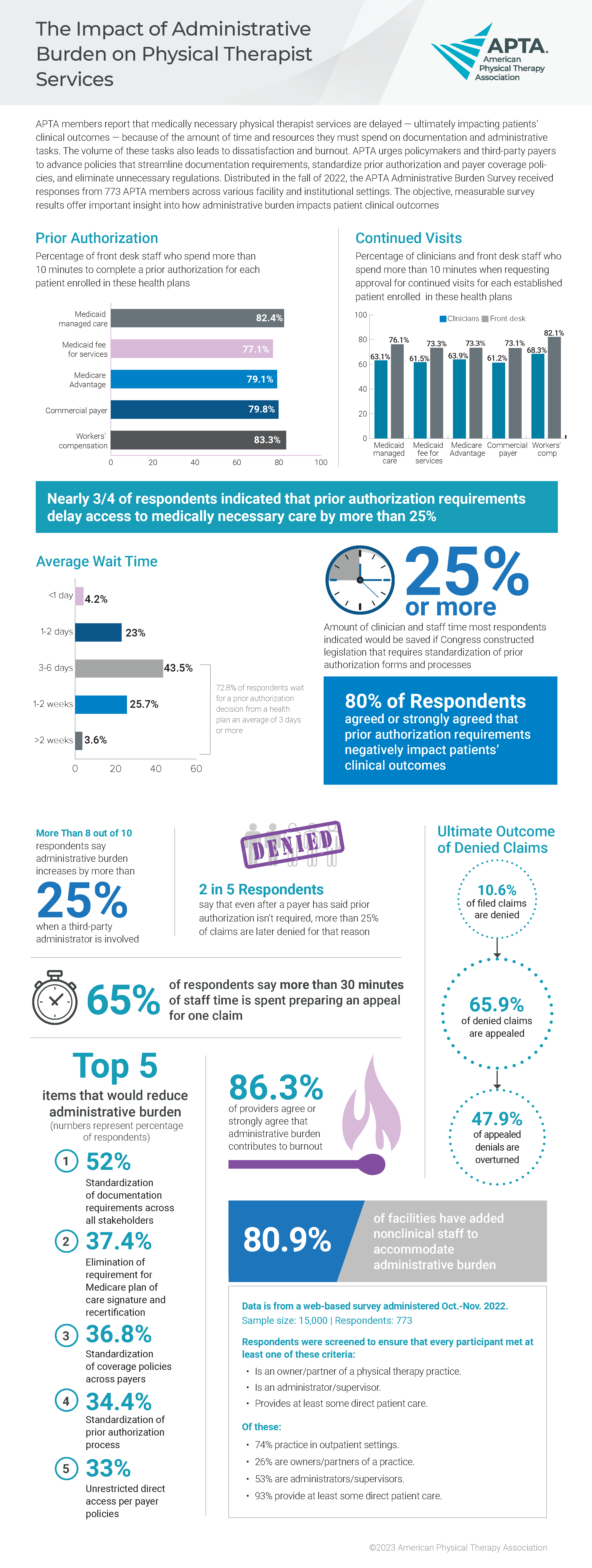
Health insurance carriers engage in a process known as “utilization review” or “prior authorization” which is a system where the carrier reviews a practitioner’s request that a patient receive a certain health care service to determine if the service is medically necessary.
This legislation would reform prior authorization by:
APTA MARYLAND